Volume: 13 Issue: 3
A Cross-Sectional Study on the Prevalence of Insomnia Among Medical Undergraduates
Year: 2025, Page: 143-147, Doi: https://doi.org/10.47799/pimr.1303.25.11
Received: May 30, 2025 Accepted: Sept. 19, 2025 Published: Dec. 30, 2025
Abstract
Background: Insomnia is defined as a persistent difficulty with sleep initiation, duration, or consolidation that occurs despite adequate opportunity and circumstances for sleep and results in concern, dissatisfaction, or perceived daytime impairment, such as fatigue, decreased mood or irritability, general malaise, or cognitive impairment. Medical students comprise a small group of people who seem to be more prone to sleep deprivation and poor sleep quality, hence, they have been considered in this study. Objectives: 1. To study the prevalence of insomnia among medical students. 2. To determine the severity of insomnia affecting medical students. 3. To determine the common factors causing insomnia in medical students. Methods: A cross-sectional study was carried out among 242 medical undergraduates of Gandhi Medical College, Secunderabad, Telangana. The Insomnia Severity Index was used to determine the severity of insomnia among medical undergraduates. Data analysis was done with the help of MS Excel, and the results were calculated. Results: Among the 242 students,11 (4.54%) were found to be insomniac, 79 (32.64%) were found to have subthreshold insomnia, and 152 (62.82%) were found to be non-insomniacs. Conclusion: This study concludes that insomnia is commonly observed among medical undergraduates, with increased screen time and higher caffeine intake identified as key contributing factors. Other demographic and lifestyle variables showed no significant association with insomnia.
Keywords: Caffeine, Exercise, Insomnia, Screen time, Sleep
INTRODUCTION
Sleep is one of the most important pillars of human health.1 Healthy and adequate sleep is necessary for proper physical and mental health, emotional and social functioning. 2
According to Roth T et.al 3 Diagnostic criteria for Insomnia is associated with following features 1. Difficulty falling asleep, staying asleep or nonrestorative sleep 2. This difficulty is present despite adequate opportunity and circumstance to sleep 3. This impairment in sleep associated with daytime impairment or distress 4. This sleep difficulty occurs at least 3 times per week and has been a problem for at least one month. Hence the above criteria were considered as operational definition for identification of study subjects. The insomnia severity index which assesses difficulty falling asleep, staying asleep, waking up too early was used to evaluate insomnia among the study population.
According to studies, 25% of the adults suffer from insomnia across several countries in Europe, whereas in India 18.6% of South Indians 4 and 28.1% of North Indians suffer from insomnia. Medical students are one of the subgroups of general population. 5
Sleep experts agree that 6 to 10 hours of sleep per 24-hour period is required for the majority of adults. The tolerated minimum sleep time is approximately 6 hours.6 Good sleep is essential for optimal neuro-cognitive and psychomotor performance as well as physical and mental health.7 Poor sleep is highly correlated with poor academic performance and reduced ability of learning. 8, 9
While previous research has explored the combined aspects of insomnia, including its prevalence, severity, and contributing factors, this study adds to the literature by specifically examining these elements among medical undergraduates.
MATERIAL & METHODS
This cross-sectional study was conducted from May 2024 to July 2024 and was approved by the institutional ethical committee, Secunderabad.
Based on study done by Aggarwal D et al 10 The sample size was estimated for the overall prevalence of insomnia p = 0.264, d = 0.06 (absolute precision) and Z = 1.96 (95% confidence) using the single-proportion formula and allowing for a 10% non-response rate, the required sample size was 231. In the present study, 242 participants were included. Convenience sampling was used and, because participants were selected by availability rather than by a probability design, no design effect was applied. Study Population: Medical undergraduates of Gandhi medical College. Inclusion criteria: 1. All the first and second-year students of the college were included in the study as there was a sudden shift of academics from tests being objective-oriented to descriptive writing in college, shift of student environment to UG hostel, stepping into adulthood from adolescence peer pressure emerges as a significant factor influencing risk behaviour and identity development 2. Students who were given consent were included in the study. Exclusion criteria:1. Students who had been diagnosed with depression and anxiety, PCOS, Diabetes and thyroid problems 2. Students who were absent on 3 consecutive visits for data collection were excluded. Anonymity and confidentiality were maintained. A semi structured questionnaire was created using google forms and sent to the students, 242 responses were collected.
Information related to demographic details, exercise obtained in a day, screen time (TV, laptop, mobile, etc) in a day and before bed, personal habits such as drinking alcohol and smoking and their frequency in a week, quantity of caffeine intake in a day was collected. Information related to the frequency of getting angry over trivial things was also collected.
Screen time less than 4 hours and screen time before bed less than 2 hours considered as moderate risk and screen time more than 4 hours and screen time before bed more than 2 hours was considered high risk among study participants. 10 Caffeine intake <2 cups of coffee/ tea in a day ( < ~177 mg/day) considered as moderate risk and >2 cups of coffee/ tea in a day ( > ~177 mg/day) considered as high risk among study population. 11
Insomnia Severity Index was used to diagnose and determine the severity of insomnia with 86.1% sensitivity and 87.7% specificity (Cronbach α = 0.91). 12 It is a seven-item questionnaire where the questions were answered based on their experiences. The dimensions evaluated were: severity of sleep onset, sleep maintenance, and early morning awakening problems, sleep dissatisfaction, interference of sleep difficulties with daytime functioning, noticeability of sleep problems by others, and distress caused by the sleep difficulties. A 5-point Likert scale was used to rate each item (e.g., 0 = no problem; 4 = very severe problem). The total score ranges from 0 to 28. The scale was 0-7=No clinically significant insomnia, 8-14=subthreshold insomnia, 15-21=moderate clinical insomnia and 22-28=severe clinical insomnia. 13
The data was processed in Microsoft Excel 22 and analysed by Chi square test using SPSS version 2023 with p value less than 0.05 were considered to be significant.
Ethical consideration
The research proposal has the approval of the Gandhi Medical College, Secunderabad, Research Ethics Committee (IEC/GMC/2024/05/025) on May 06, 2024.
RESULTS
A total of 242 students participated in the study, belonging to the age group of 17-24. The mean age was 18.39 years. 100 (41.3%) students were male, and 142 (58.6%) students were female.
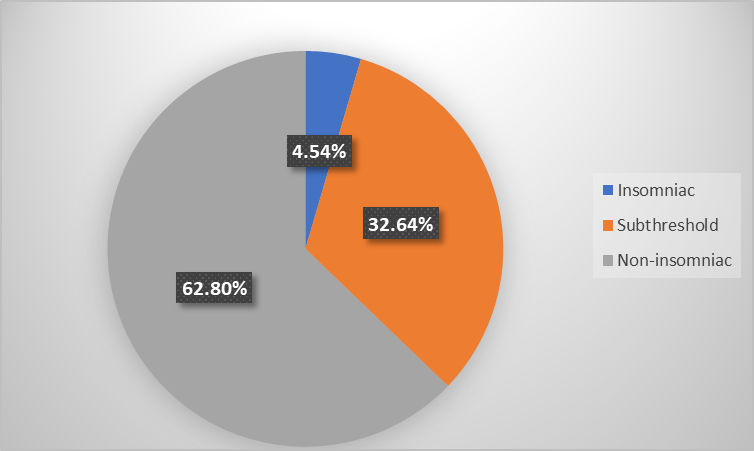
Figure 1: Prevalence of insomnia status among medical undergraduates
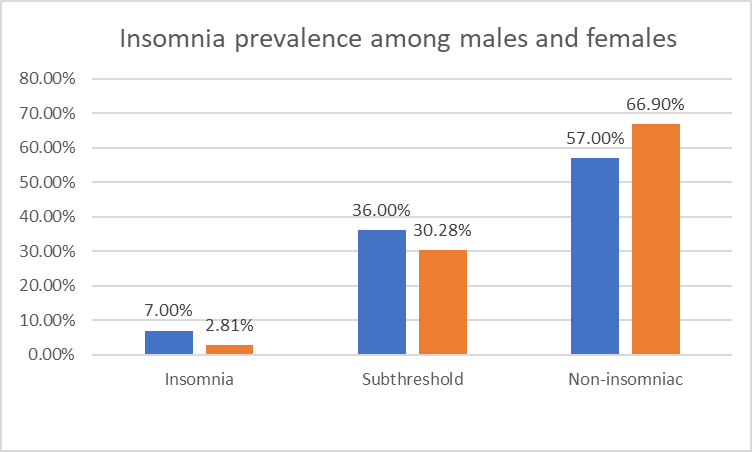
Figure 2: Prevalence of Insomnia among males and females
Table 1: Association between Demographic characteristics, associated lifestyle factors and Insomnia status
|
|
Total (242) |
Non-insomniacs (152) |
Subthreshold insomniacs (79) |
Insomniacs (11) |
p value |
|
SEX |
|
|
|
|
|
|
Male |
100 (41.3%) |
57 (37.5%) |
36 (45.6%) |
7 (63.6%) |
0.152 |
|
Female |
142 (58.7%) |
95 (62.5%) |
43 (54.4%) |
4 (36.4%) |
|
|
AGE |
|
|
|
|
|
|
≥ 19 years |
86 (35.5%) |
51 (33.6%) |
29 (36.7%) |
6 (54.5%) |
0.141 |
|
<19yrs |
156 (64.5%) |
101 (66.4%) |
50 (63.2%) |
5 (45.5%) |
|
|
SCREEN TIME IN A DAY |
|
|
|
|
|
|
≤ 4 hrs |
78 (32.2%) |
62 (40.8%) |
15 (19%) |
1 (9%) |
0.003 |
|
>4hrs |
164 (67.7%) |
90 (59.2%) |
64 (81%) |
10 (91%) |
|
|
SCREEN TIME BEFORE BED |
|
|
|
|
|
|
≤ 2hrs |
208 (85.9%) |
135 (88.8%) |
64 (81%) |
9 (81.8%) |
0.25 |
|
>2hrs |
34 (14.1%) |
17 (11.2%) |
15 (19%) |
2 (18.1%) |
|
|
EXERCISE |
|
|
|
|
|
|
≥30 minutes |
60 (24.8%) |
38 (25%) |
21 (26.6%) |
1 (9%) |
0.559 |
|
<30minutes |
182 (75.2%) |
114 (75%) |
58 (73.4%) |
10 (91%) |
|
|
CAFFEINE |
|
|
|
|
|
|
<2 cups of coffee/ tea in a day |
211 (87.2%) |
137 (90.1%) |
66 (83.5%) |
8 (72.7%) |
0.05 |
|
≥ 2 cups of coffee/ tea in a day |
23 (9.5%) |
12 (7.9%) |
8 (10.1%) |
3 (27.3%) |
|
|
Other forms of caffeine intake |
8 (3.3%) |
3 (2%) |
5 (6.3%) |
0 (0%) |
|
|
ALCOHOL |
|
|
|
|
|
|
No, occasional |
240 (99.2%) |
152 (100%) |
79 (100%) |
11 (100%) |
0.067 |
|
<4 times a week, >4 times a week |
2 (0.8%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
|
SMOKING |
|
|
|
|
|
|
<10 cigarettes per week |
241 (99.9%) |
152 (100%) |
78 (98.7%) |
11 (100%) |
0.112 |
|
>10 cigarettes per week |
1 (0.1%) |
0 (0%) |
1 (1.3%) |
0 (0%) |
|
According to Figure 1, it was seen that 11 (4.54%) had clinical insomnia, 79 (32.64%) were having subthreshold insomnia and 152 (62.8%) were non-insomniacs.
From the Figure 2 it was seen that 7% (7) of the males and 2.81% (4) of the females were suffering from insomnia whereas 36% (36) of the males and 30.28% (43) of the females were suffering from sub threshold insomnia among study population. 57% (57) and 66.9% (95) were found to be Non insomniacs.
According to Table 1, this study found no statistically significant difference in insomnia prevalence between males and females (p-value = 0.152). Age did not significantly influence insomnia status (p-value: 0.141), and no clear pattern was observed between age groups. A highly significant association was found between increased daily screen time (>4 hours) and higher rates of insomnia (p-value: 0.003). However, screen time before bed showed no significant link to insomnia (p-value: 0.25). Exercise duration was not significantly associated with insomnia (p-value: 0.559). Caffeine intake showed a marginally significant association with increased insomnia risk (p-value: 0.05). Alcohol and smoking were found to be non-significant.
DISCUSSION
It has been seen in this study that 4.54% and 32.64% of the students of Medical Undergraduates, Secunderabad, Telangana suffer from clinical insomnia and subthreshold insomnia respectively while 62.8% of the students are non-insomniacs. This is slightly different from the findings of Shakeel HA et al. 14 in their study conducted in 2019 where 40.74% of the students were reported as insomniac.
Our study found higher insomnia prevalence among males, differing from Boer J et al. 15 who reported higher rates in females. However, Shakeel HA et al. 14 found no significant gender difference, and Wong et al. 16 noted that academic and lifestyle factors can vary by setting, potentially explaining population-specific patterns.
The major factor causing insomnia is seen to be increased screen time in a day. The percentage of students suffering from both insomnia and subthreshold insomnia increases with increase in screen time in a day. 10 out of the 11 insomniac students have greater than 4 hours of screen time in a day and 67 out of the 83 students with subthreshold insomnia have greater than 4 hours of screen time in a day. This finding is consistent with the findings of White AG et al. 17 from their study on the influence of mobile phones on sleep quality where they established that increased screen time is leading to decreased sleep quality.
In comparing the study by Shakeel HA et al. 14 with the provided results, we see that males tend to have higher insomnia rates (both clinical and subthreshold), and this difference is statistically significant. Females, on the other hand, show a lower prevalence of insomnia and a higher percentage of non-insomniacs. Screen time and caffeine consumption appear to play key roles in insomnia prevalence, and their effects may be more pronounced in males.
Daily screen time was significantly associated with insomnia, but bedtime screen use was not (p = 0.25). Similar findings in medical student cohorts from the study Wong et al. 16 suggest that the content and context of screen use, as opposed to timing alone, may influence sleep quality, contrasting with general population studies done by White AG et al. 17
Caffeine intake showed only a marginal association with insomnia (p = 0.05), whereas Chaudhary et al.11 found a clear link between high caffeine consumption and sleep disturbances. The weaker association in our study may be due to moderate consumption patterns or individual tolerance differences.
Similarly, exercise, and substance use (alcohol, smoking) did not significantly impact insomnia. Low reporting rates and healthy lifestyle choices commonly seen among medical students, as also noted by Wong et al. 16, may have contributed to these non-significant findings.
CONCLUSION AND RECOMMENDATIONS
This study found that clinical insomnia affected 4.54% of medical undergraduates, while 32.64% had subthreshold insomnia, indicating that a substantial proportion experience some degree of sleep disturbance. Increased daily screen time and higher caffeine intake were the main associated factors, whereas other lifestyle and demographic variables showed no significant association. These findings support the promotion of healthy sleep habits, reduced screen exposure, and moderated caffeine use. We recommend regular screening using validated tools such as the Insomnia Severity Index (ISI) at least once per academic year during routine health check-ups, with students scoring in the clinical range referred to campus health services or a mental health professional for further evaluation and management.
Limitation
As participants may not accurately report behaviours like screen time or caffeine intake there is a chance of recall and social desirability biases. Although participants with depression, PCOS, and thyroid disorders were excluded, uncontrolled factors like obstructive sleep apnoea or undiagnosed anxiety were not excluded because screening for them was beyond the scope of the study and may have influenced the observed prevalence and severity of insomnia. The use of a convenience sampling technique introduces potential sampling bias, as the sample may not be fully representative of all medical undergraduates, potentially limiting the external validity of the findings. There is a limited generalizability as study sample was limited to first- and second-year medical students.
Disclosure
Acknowledgement
We would like to express our profound gratitude to the medical students of Gandhi Medical college for their contributions to the completion of this project.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
-
Islam, Zohurul, Hsan, Kamrul, Islam, Saiful, Gozal, David & Hossain, Mahfuz . 2021. Assessment of sleep quality and its association with problematic internet use among university students: a cross-sectional investigation in Bangladesh. Sleep Science 14(S 01):8–15.
-
Babicki, Mateusz, Piotrowski, Patryk & Mastalerz-Migas, Agnieszka . 2022. Assessment of Insomnia Symptoms, Quality of Life, Daytime Sleepiness, and Psychoactive Substance Use among Polish Students: A Cross-Sectional Online Survey for Years 2016–2021 before and during COVID-19 Pandemic. Journal of Clinical Medicine 11(8):2106.
-
Roth, T . 2007. Insomnia: Definition, Prevalence, Etiology, and Consequences. Journal of Clinical Sleep Medicine 3(5 suppl):S7–S10.
-
Panda, Samhita, Taly, Arun B, Sinha, Sanjib, Gururaj, G, Girish, N & Nagaraja, D . 2012. Sleep-related disorders among a healthy population in South India. Neurology India 60(1):68–74.
-
Sen, M K, Adhikari, Tulsi & Suri, J C . 2008. Epidemiology of Sleep Disorders in the Adult Population of Delhi: A Questionnaire Based Study. Indian Journal of Sleep Medicine 3:128–137.
-
Ferrara, Michele & Gennaro, Luigi De . 2001. How much sleep do we need? Sleep Medicine Reviews 5:155–179.
-
Giri, PA, Baviskar, MP & Phalke, DB . 2013. Study of Sleep Habits and Sleep Problems Among Medical Students of Pravara Institute of Medical Sciences Loni, Western Maharashtra, India. Annals of Medical and Health Sciences Research 3(1):51–54.
-
Campos-Morales, Rosa M, Valencia-Flores, Matilde, Castaño-Meneses, Alejandra, Castañeda-Figueiras, Sandra & Martínez-Guerrero, José . 2005. Sleepiness, performance and mood state in a group of Mexican undergraduate students. Biological Rhythm Research 36(1-2):9–13.
-
Rodrigues, Raimundo Nonato D, Viegas, Carlos A A, Silva, Aída A A Abreu e & Tavares, Paulo . 2002. Daytime sleepiness and academic performance in medical students. Arquivos de Neuro-Psiquiatria 60(1):6–11.
-
Aggarwal, D, Das, A, Krishna, Str, Hyndavi, S, Palepu, S & Kumar, S . 2024. Association between increased screen time, sedentary behavior, and insomnia among Indian adults: a cross-sectional nationwide online survey. Journal of Family Medicine and Primary Care 13(7):2761–2766.
-
Chaudhary, Ninad S, Grandner, Michael A, Jackson, Nicholas J & Chakravorty, Subhajit . 2016. Caffeine consumption, insomnia, and sleep duration: Results from a nationally representative sample. Nutrition 32:1193–1199.
-
Buysse, Daniel J, Reynolds, Charles F, Monk, Timothy H, Berman, Susan R & Kupfer, David J . 1989. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research 28(2):193–213.
-
Brown, Franklin C, Buboltz, Walter C & Soper, Barlow . 2002. Relationship of Sleep Hygiene Awareness, Sleep Hygiene Practices, and Sleep Quality in University Students. Behavioral Medicine 28(1):33–38.
-
Shakeel, Hassan Abdullah, Maqsood, Hamza, Ishaq, Asher, Ali, Basit, Hussain, Humza, Khan, Ali Raza & Shah, Syed Asfand Yar . 2019. Insomnia among medical students: a cross-sectional study. International Journal of Research in Medical Sciences 7(3):893.
-
Boer, Jolijn, Höhle, Nadya, Rosenblum, Lisa & Fietze, Ingo . 2023. Impact of Gender on Insomnia. Brain Sciences 13(3):480.
-
Wong, J G W S, Patil, N G, Beh, S L, Cheung, E P T, Wong, V, Chan, L C & Mak, F Lieh . 2005. Cultivating psychological well-being in Hong Kong's future doctors. Medical Teacher 27(8):715–719.
-
White, A G, Buboltz, W & Igou, F . 2011. Mobile phone use and sleep quality and length in college students. International Journal of Humanities and Social Science 1(18):51–58.
Copyright
©2025 (Mitnala) et al. This is an open-access journal, and articles are distributed under the terms of the Creative Commons Attribution License CC-BY 4.0. (https://creativecommons.org/licenses/by/4.0/) which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited.
Cite this article
Mitnala NV, Nayakallu L, Nakka T, Nagamalla KT, Desai N, Dayyala S, Thimmapuram RC. A Cross-Sectional Study on the Prevalence of Insomnia Among Medical Undergraduates. Perspectives in Medical Research. 2025;13(3):143-147 DOI: 10.47799/pimr.1303.25.11